Medical workers at Fairbanks Memorial Hospital say the hospital’s capacity is being strained by high COVID-19 rates, and the community should be more alarmed. The hospital is receiving a surge in patients from the Fairbanks North Star Borough but also from Delta Junction and those diverted from Bassett Hospital on Fort Wainwright.
Medical executives gave a report to Greater Fairbanks Community Hospital Foundation Board on Friday, saying they are demoralized by the lack of community response, even as the disease becomes more preventable.
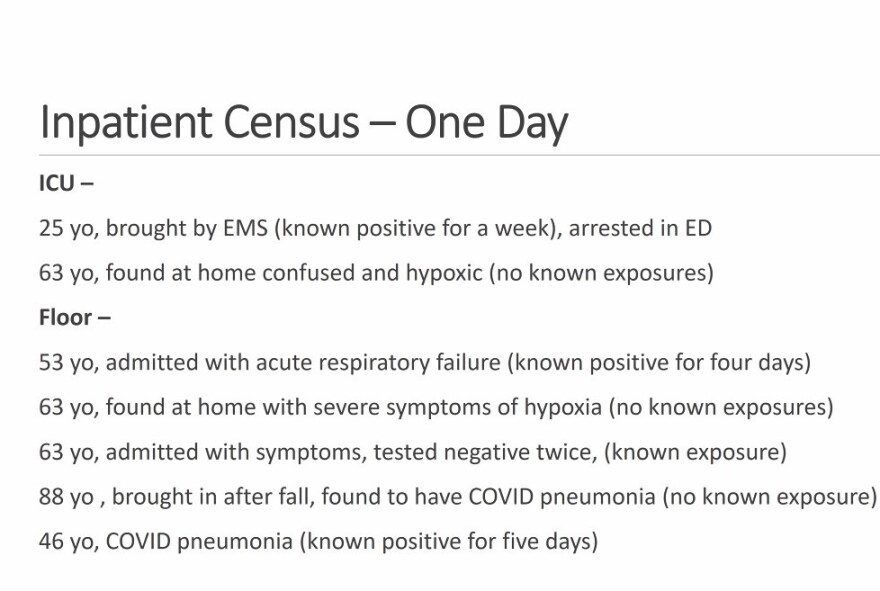
The hospital is reporting record high admissions of coronavirus disease – even more than the surge last November. About 18% of the admissions at Fairbanks Memorial Hospital have COVID-19.
Dr. Barbara Creighton, who has been attending many of them, says the surge is preventable.
“There is the disconnect. You know, we have businesses opening, school buses flying, restaurants going, and we have visitors happening, and yet we have our highest case rates. And so, we are like does anybody see this? This place is on fire with COVID.”

People hospitalized for COVID in the last year were generally elderly, and many died. But that demographic is nearly 70% immunized in the state, so fewer elderly Alaskans are getting sick.
The patients admitted in the last weeks are younger and they are not fully vaccinated.
“It’s really coming fast now. And that is the most worrisome thing for me, because this is a different demographic; these are young people cardiac-arresting before they come into the hospital. These are middle-aged white guys. I’m sorry to say that. But it really is that demographic that hasn’t gotten around to getting vaccinated, or doesn’t really feel like they need vaccination, and they want to see what the vaccine is going to do before they take it. Those are the people we are seeing come in with COVID.”
Shelly Ebenal, the CEO of Foundation Health Partners, the non-profit that runs the hospital, says the staff is working through a change in patient response.
“This new group of patients, some of these folks, some -- these are generalizations, so be careful with that -- some of these folks are folks that are anti-vaxxers or anti-maskers, and they don’t believe that they have COVID, or are sick because of it, and our staff is getting some very angry folks.”
When you see our staff members, please tell them 'thank you.' They really need that right now; our morale is really low.
Dr. Creighton says treatments have changed; the “workhorse therapy” has become high-flow oxygen and non-invasive ventilation where there is no tube down the patient’s airway and they can eat and talk.
But treatment is still only supportive– there is no cure for COVID-19. There is just a long wait while each patient’s lungs recover.
“And we are seeing them stay longer, because they are not dying. They are actually staying for two, three weeks and turning around, which I’ve never been more proud of. You know, this could be our finest hour.”
She says the hospital is running out non-invasive ventilators as patients fill up the COVID wing.
Dr. Angelique Ramirez, Chief Medical Officer, for Foundation Health Partners, says a month ago the hospital had several days with no COVID-19 patients at all. Now the urgent care walk-in at Tanana Valley Clinic, as well as FMH Emergency Department are seeing several COVID patients each day, and at the hospital 10 to12 folks are in COVID beds each night -- the entire second floor of the south wing is only COVID patients.
“I don’t know that we’ve had such a dramatic change in one month before.”
Ramirez reported to the Foundation Board how younger people are spreading the disease faster. She says right now the borough has a testing positivity rate of almost 10%.
“This is the highest it’s ever been, you can see that it’s a sharp uptick. And what this tells us is that we are not capturing, by testing, everybody who is positive. The challenge is, if they don’t know that they’re sick, they are out in the community spreading it.”

Ramirez says confidence and hope comes from the difference in factors present now, that weren’t part of the equation last November. She says 70% of the FHP staff is vaccinated, unlike last November and December when many were sick at home or quarantining because they had been exposed to someone with COVID-19. Also different, is other Alaska hospitals can take patients from the Interior if FMH becomes overwhelmed.
“So we are in a hotspot. Everyone else has capacity, so that’s nice to know that other places have capacity. But the reality is still we are the only hospital in the Interior.”
CEO Shelly Ebenal says the hospital staff is deflated by the surge in patients and the community not taking easy measures to fend off what has become preventable.
“They are still in full COVID mode. I know our community is tired, I know they don’t want to mask. They want this to be over, but it’s not. When you see our staff members, please tell them ‘thank you.’ They really need that right now; our morale is really low. They feel like they are not being appreciated for their work, because they are in the thick of it right now.”